- Dry socket can happen when a tooth is extracted but fails to heal normally.
- It most commonly develops in the empty socket of extracted wisdom teeth.
- Your dentist can take certain precautions but prevention largely rests on your shoulders.
- There are many simple measures you can take to lower your risk of dry socket.
Usually, recovering from having a tooth extracted goes off without a hitch, but occasionally – about 1-4% of the time – patients go on to develop a complication called alveolar osteitis, also known as dry socket.
When the empty socket doesn’t heal properly, pain, headache, spasms and swelling can develop.
Here we outline the steps you can take to help the healing process to proper completion.
What exactly is dry socket?
Having your wisdom teeth pulled is almost a rite of passage into young adulthood. According to the American Public Health Association, some 10 million wisdom teeth are removed each year.
Of course, wisdom teeth aren’t the only ones that may require removal. The Centers for Disease Control and Prevention note that by age 50, we lose an average of 12 teeth. Among adults 65-74 years of age, some 26% have no teeth at all.
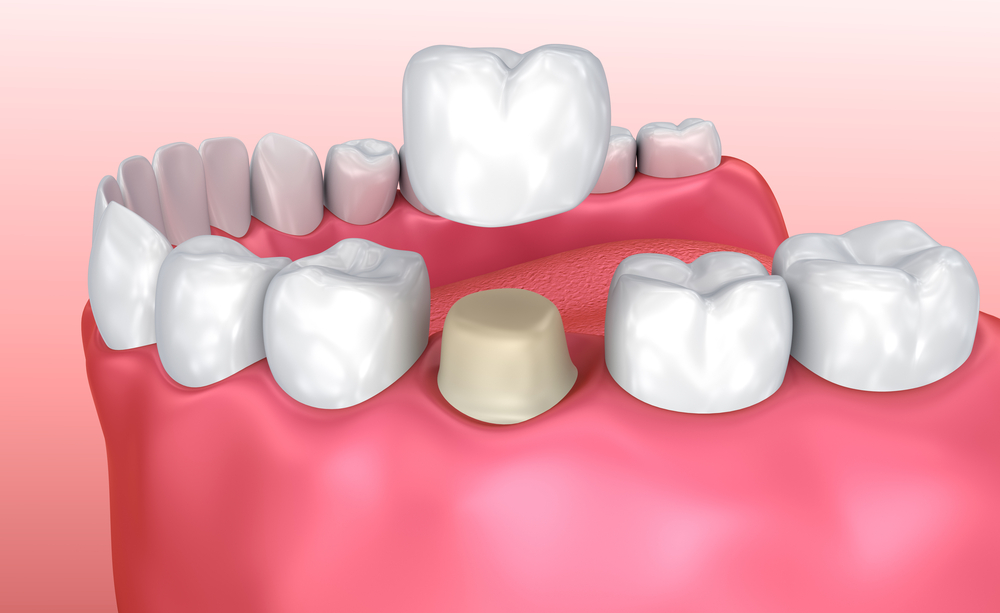
Dry socket is a painful condition that may develop 1-3 days after a tooth is removed. The condition is related to the breakdown or loss of the clot that normally covers and protects the socket where the tooth used to be.
This clot is essential as it provides the foundation for new bone growth as well as for the development of soft tissue over the clot.
Consequences of clot loss
When the clot is lost or disturbed, it leaves the bone and nerves at the site exposed. When proper healing is disrupted, serious pain, bad breath and possibly a bad taste in the mouth can develop. The socket becomes inflamed and can fill with food matter, adding to the pain.
Also, the intense pain signals may stimulate nerves extending from the jaw toward the ear and neck. Unfortunately, this pain doesn’t respond to over-the-counter painkillers.
In addition, headache, insomnia, dizziness, jaw muscle spasms and swelling of local lymph glands are also common features of the condition.
Predisposing factors
Dry socket is 10 times more common when the tooth is impacted and has to be surgically removed. It is also more likely when the tooth involved is in the lower jaw.
Other predisposing factors include the patient’s age – it’s more common among those over 45 years old. It is also more common among women, especially those using oral contraceptives.
Finally, if you’ve had dry socket in the past, it is more likely to reoccur with future extractions.
Treating dry socket
Treatment for dry socket is aimed at alleviating the symptoms, which essentially breaks down to analgesics for pain and mouthwash for odor or taste. Attempts may also be made to restart the healing process.
Dr. Zach Christopherson who practices dentistry in Cheyenne, WY, notes that “Generally, the area is anesthetized. The socket is then cleaned of debris and rinsed with a saline solution. There are also medications used – frequently a paste, for example – specifically for treating dry socket.”
Since dry socket is not an infection, it isn’t usually treated with antibiotics. “However, a secondary infection can occur that may need antibiotics,” Dr. Christopherson points out. Medicated dressings (e.g. Alvogyl) are changed daily until pain subsides and healing begins. Anti-inflammatories like aspirin or ibuprofen are usually used as well.
An ounce of prevention
Some of the risk factors for dry socket are out of your control but there are steps you can take to lower your chances of developing this condition. We outline these measures in this section.
- Stop smoking
Avoid tobacco products for several days before the procedure as they can slow healing.
A study that looked at 4,000 wisdom tooth removals found patients who smoked a half-pack of cigarettes a day had a 4- to 5-fold increase in dry socket when compared to nonsmokers.
Among those patients smoking a pack a day, more than 20% experienced dry socket, which went up to 40% among those who smoked on the day of the procedure itself.
- Advise your dentist of your meds
If you are using birth control pills, make sure you discuss this with your doctor beforehand, as they can affect the blood’s ability to clot properly.
In fact, you should make sure your dentist has a good idea your current health status before the procedure. Share information about any medical conditions you may have as well as any associated medications, supplements or other treatments you’re taking at the time.
- Practice good oral hygiene
Good oral hygiene can also lessen the chances that harmful bacteria will interfere with healing. A pre-existing infection in the mouth can prevent the blood clot from forming properly following removal of the tooth.
Also, some bacteria are known to specifically break down clots.
Following your dentist’s advice
Failing to follow the home care advice of your dentist following the extraction may increase the risk of dry socket as well. Typical post extraction instructions include:
- Pressing on the gauze packing for one hour
- Avoiding hot food on the day of extraction
- Limit chewing on the extraction site
- Don’t put your tongue or finger inside the socket
- Avoid rinsing your mouth or using a straw for the next 24 hours
- Don’t smoke or consume alcohol for the next 24 hours
- Avoid performing strenuous activities for the next 3 days.
Dr. Christopherson sums up: “Patients should keep three ‘S’ words in mind after tooth extraction: do not smoke, spit or suck after having a tooth pulled. Smoking delays healing and is likely the most common cause of dry socket. Spitting and sucking – using a straw, for example – both put negative pressure on the blood clot, which can remove it from the socket and cause dry socket to occur.”
Trauma or difficulty during tooth extraction also increases the likelihood of dry socket, so it would be prudent to avoid waiting until you’re in dire straits before scheduling the procedure.
Again, this falls into the category of taking good care of your oral health, including having regular dental care checkups. Inexperienced professional care has also been cited as a cause of dry socket. This one may be out of your control but it’s worth noting so you can ask the right questions when choosing your dentist.
What the dentist may do to lower your risk
There is reliable evidence that using an antiseptic rinse just before the procedure, and/or packing the extraction site with antiseptic gel after the tooth is extracted will decrease the risk of dry socket.
Other steps your dentist may take include prescribing antibiotics, especially if you have a chronic health condition or your immune system is compromised.
Remember, a certain amount of pain following a tooth extraction is normal and can be expected. However, it should gradually diminish with time.
If you experience increasing pain in the days following a dental extraction, don’t hesitate to consult your dentist as soon as possible.
Simple steps lead to smooth sailing
Tooth removal is never fun but putting in the effort to help your procedure go smoothly will help you avoid any of the post-extraction pitfalls, such as dry socket.
Taking the simple steps outlined here for pre- and post-care will help you avoid a long and painful road to recovery.
If you are concerned about dry socket, Dr. Christopherson has this to say: “Dry socket can be very painful but it is not life threatening. A follow-up visit with the dentist who did the surgery is usually free and may relieve you of your concerns, even if not all of the pain.”