Varicose veins are a common condition in both men and women, and though we more readily associate them with old age, younger adults can get them too.
Not only are these enlarged blood vessels in the lower leg unflattering, but they also cause discomfort and pose serious health risks. Regardless of whether or not you experience pain, the appearance of varicose veins can lead to feelings of insecurity. Therefore, people often have them removed for cosmetic reasons.
What are varicose veins?
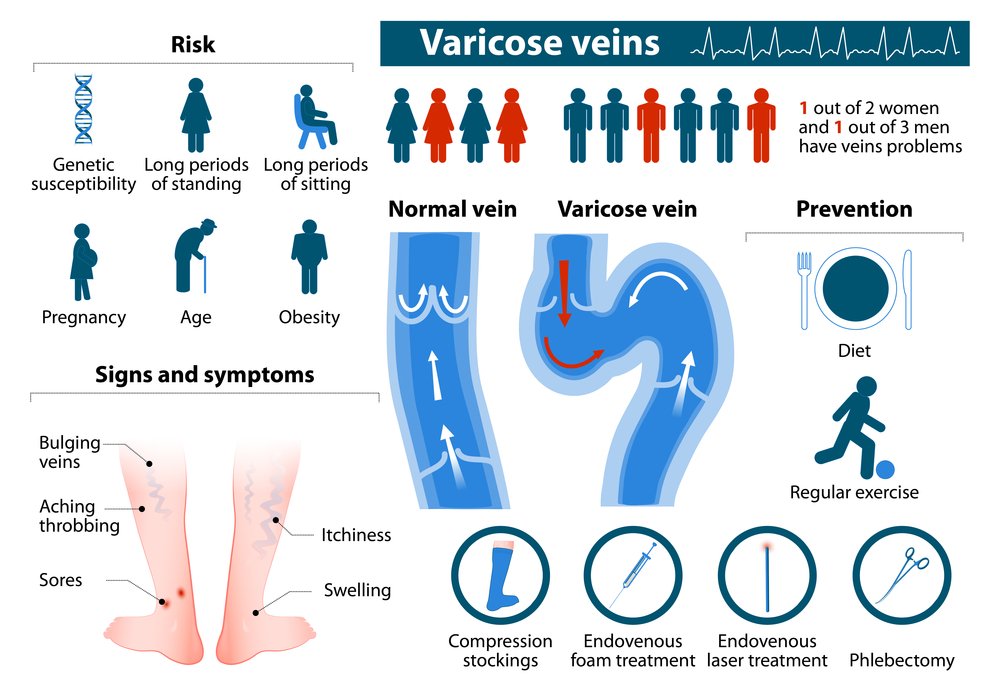
Being that varicose veins affect normal veins, they are considered a vascular condition. Normal healthy veins have valves that assist the process to return blood flow from the legs back to the heart. With varicose veins, the theory is that there is either damaged or weakened valves, or weakness in the vein wall that causes a physical malfunction known as venous insufficiency, venous stasis or venostasis.
“Venous stasis occurs when the valves in the veins, which help the blood return back to the heart, start to fail and leak,” says New York plastic surgeon Dr. Anthony Taglienti. “As a result, blood pools, and the result is enlarged veins. Sometimes, a part of the venous system may be completely blocked; this will also lead to varicose veins. Typically patients with this issue have unilateral leg swelling, and experience pain at the end of the day.”
Varicose veins are not to be confused with deep vein thrombosis (DVT), a more serious condition that occurs when a blood clot forms in one or more of the deep veins in the legs. DVT can happen if you don’t move for a long time, such as after surgery or following an accident, causing blood clots to block the blood flow in the lungs (pulmonary embolism).
Symptoms of varicose veins
For the most part you will experience dark veins, usually a blueish/purple color. They may look swollen and lumpy.
Other symptoms could include:
- Heavy, aching legs
- Excessive bleeding (after injury) in the affected area
- Swollen ankles
- Dry skin or eczema
- Constant leg cramps
- Spider veins in the affected area
- Atrophie blanche – a whitish scar developing on the lower leg or foot from poor blood flow after injury
Causes of varicose veins
Blood travels from the heart to different areas of your body through one way vein valves. If the vein walls become elastic and less flexible, blood may begin to leak backward and flow in the opposite direction. When this occurs you can end up with a swollen vein, or varicose vein. Usually veins that are furthest from the heart are most likely to be affected. This is why a lot of the time varicose veins are found in the legs and/or feet area.
Risk factors for varicose veins
Varicose veins can occur in almost anyone, at any age, though higher risk factors include:
- Family history/ genetics – most common
- Age – the older we get the more susceptible we become
- Women – progesterone levels can increase risk
- Obesity – due to increase in venous pressure
- Pregnancy – due to physical and hormonal changes
- Sitting or standing still for long periods – due to changes in venous stress and pressure
Diagnosis of varicose veins
Though varicose veins are usually fairly obvious, your doctor will reach a diagnosis by palpating the veins and examining the skin discoloration and texture of your legs while you are sitting and standing. You will also be asked questions about your family history, and asked to describe any other symptoms you might have such as heaviness, tiredness in the legs, swelling, cramps, tingling, itching, numbness and pain.
“Larger varicose veins should be examined with a Doppler ultrasound before treatment, to be sure that they are in fact ‘extra’ vessels that are not actively carrying blood to the heart/larger feeder vessels,” says Beverly Hills dermatologist and university clinical instructor Dr. Tsippora Shainhouse.
Once a diagnosis has been reached, your doctor will then discuss the range of treatment options available.
Varicose vein treatment options
“There are multiple treatment options available, depending on the patient’s anatomy, other medical problems and personal preferences,” says general surgeon Dr. Brian Heeringa of Northern Michigan.
Compression
Compression stockings are often a first line therapy for varicose veins.
Dr. Heeringa informs that trying compression for a period of time is often an insurance company requirement before they will cover treatment of varicose veins.
Sclerotherapy
Sclerotherapy involves the use of chemicals injected into the varicose veins, which subsequently causes them to shrink, scar up and gradually disappear over a number of weeks. “Common chemicals used in the United States include hypertonic saline and sodium sotradecol. Foam versions work best for larger, blue varicose vessels,” says Dr. Shainhouse.
After the procedure, “you should continue to wear compression stockings for two months, to make sure that the veins do not re-open,” adds Dr. Shainhouse. You may also need subsequent treatments for larger varicose veins.
Laser ablation
“While external laser treatments can help treat dark purple veins and blue veins through the skin, it is most effective to guide a laser into a vessel through a fiber-optic wire and zap them from the inside,” says Dr. Shainhouse. This is known as endovenous laser treatment, an image-guided method that “causes the vessel wall to collapse and scar down and is eventually broken down by the body,” informs Dr. Shainhouse. Endovenous laser treatment is conducted with local anesthetic.
VenaSeal
“VenaSeal is the latest treatment option,” says Dr. Shainhouse. “It involves the injection of a medical-grade adhesive that literally shuts the varicose veins permanently. It can usually be performed in one session.” This treatment involves a number of needle sticks into the vein and is performed with a local anesthetic to minimize any pain or discomfort.
Vein Stripping
“Varicose veins can be physically removed from the legs by making tiny serial incisions in the overlying skin and pulling them out,” says Dr. Shainhouse. “This surgical treatment is best for painful, bulging, large veins. It is usually performed by a vascular surgeon, but some dermatologic surgeons will perform this as well.”
Vein stripping is one of the oldest techniques for varicose vein removal. Since there are more advanced treatments available today, Dr. Heeringa informs that “traditional stripping is generally a thing of the past.”
Are there side effects or downsides to the treatment choices?
Dr. Taglienti informs that “with more invasive procedures, like phlebectomies, there can be swelling, bruising, and discomfort. With the more superficial veins, some slight discomfort and bruising can occur.”
“All medical procedures carry some risk, but treatments for varicose and spider veins are very safe and can typically be done in the office with little or no interruption in normal activities,” says Dr. Heeringa. “I would recommend that any prospective patients discuss the advantages, risks, benefits and alternatives to any treatment options with their physician so that they can choose the procedure that fits them and their anatomy best.”
Does pregnancy cause varicose veins?
Unfortunately, approximately 9.4 percent of women acquire varicose veins during pregnancy.
“Pregnancy increases the risk for varicose veins for several reasons,” says Dr. Heeringa. “First of all, during pregnancy there is an increase in the amount of blood a mother has in her vascular system to help support the growing baby and secondly the growing uterus can compress the veins in the pelvis which obstructs the flow out of the legs leading to further distention of the leg veins. Finally, progesterone, one of the female hormones, causes the veins to be more elastic.”
Are spider veins and varicose veins the same?
“Spider veins are tiny blue or red veins on the surface of the skin, while varicose veins are larger, ropy and twisty veins,” says Dr. Heeringa. “Varicose veins are typically considered a medical problem. Spider veins tend to be more of a cosmetic concern. Having said that, patients being treated for varicose veins often experience not only a dramatic improvement in their symptoms but also in the appearance of their legs.”
“Spider veins and varicose veins are usually part of the same problem – venous stasis,” adds Dr. Taglienti. “In that sense, the two issues are related. However, the treatments differ and the reason for this is really based on the caliber or size of the veins being treated; smaller veins typically respond better to sclerotherapy and laser, while larger veins are not amenable to these types of treatments.”
How can varicose veins be prevented?
“Currently there is nothing guaranteed to prevent varicose veins but avoiding risk factors can help minimize one’s the odds,” says Dr. Heeringa. “We recommend maintaining a healthy weight, and an active lifestyle.”
Dr. Shainhouse informs that exercises like walking, swimming and flexing the leg muscles help because these recruit the calf and thigh muscles surrounding the vessels to help push the blood through them. This helps prevent pooling and stretched out vessels.
Further to this, Dr. Heeringa suggests that high heels should be avoided or their use minimized as much as possible, as wearing them limits the pumping action of the calf and increases your risk of developing varicose veins.
Additional prevention methods include elevating the legs when seated and wearing compression stockings during the day, especially if you work in a profession where you’re on your feet for long periods of time – healthcare workers, hairdressers, teachers, chefs and such. Just remember to remove the compression garments at bedtime.









