Plastic and reconstructive surgeons often play a critical role in transforming the lives of people who have been victims of unfortunate accidents, such as burn injuries. Fortunately, there are a number of procedures surgeons can use to assist with the physical and cosmetic limitations of burn-damaged skin, vastly improving their patients’ quality of life.
Being a burn victim can have significant health impacts. Not only do burn patients have to live with possible physical limitations, they also face substantial emotional, social and situational challenges, especially when highly visible scars affect their physical appearance.
When asked by researchers to describe the challenges they face, burn patients cited a wide range of barriers, including self consciousness, fear of rejection, embarrassment, humiliation, and having to deal with frequent questions and comments from others. As a consequence, their social and interpersonal connections are often greatly impacted.
While it may not be possible to completely eliminate the visual appearance of burn scars, nonoperative and operative means can be used to modify or alter scar tissue to achieve both cosmetic and functional improvements. To understand more about burns and what can be done to improve them, we spoke with two burn experts – New jersey plastic and reconstructive surgeon Dr. Russell Ashinoff, and New York plastic and reconstructive surgeon Dr. Jonathan Landon.
Classification of Burns
Burns can occur due to any number of accidents where the skin is subjected to excessive heat, although flame burns are generally more severe in their depth and size.
“Burns are classified by depth of penetration through the skin into superficial (first-degree), partial thickness (second-degree) and full thickness (third-degree),” says Dr. Ashinoff. “Partial thickness is further divided into superficial and deep categories.”
Acute Burn Care
“Most deep second-degree burns and all third-degree burns require reconstructive surgery,” says Dr. Landon. “This involves split thickness skin grafting or full thickness skin grafting depending on the burned area. Burn resuscitation in the immediate post burn period (initial 24 hours) is absolutely critical.”
“Proper resuscitation of the burn patient with appropriate fluid management can prevent burn wounds from progressing to the next level. In other words, with proper hydration/ fluid resuscitation, we can prevent a superficial second-degree burn wound from converting into a deep second-degree burn wound. This would save the patient from surgical reconstruction,” says Dr. Landon.
“During the initial post-burn period, the tissue adjacent to the most badly damaged areas can be considered in a ‘state of flux.’ Proper management will prevent these areas from deteriorating and converting into deeper burn levels. With rapid, effective, and efficient management, the burn surgeon can prevent propagation of the zone of injury, lessening the total surface area requiring reconstructive efforts,” adds Dr. Landon.
Initial Burn Interventions
“Burn scarring that leaves a patient with a cosmetic deformity is treated in a staged fashion,” says Dr. Ashinoff. “Soon after the initial burn wounds are healed, silicone sheeting may be prescribed, as it’s been proven to improve long-term scar appearance. Non-surgical treatments are usually considered within the first year. These include corticosteroid injection for hypertrophic scars, and laser therapy.”
“If these measures are unsuccessful or a functional limitation develops, surgical treatment is considered. The type of procedure chosen will depend upon the area and type of scar,” adds Dr. Ashinoff.

Reconstructive Burn Surgery
After a burn has fully healed, reconstructive surgery may be necessary for cosmetic or functional purposes. Surgery is required in approximately 13 percent of burn patients, and facial reconstructive surgery is performed in approximately 5.3 percent of patients.
“Most scars require 6-12 months before they are mature,” says Dr. Ashinoff. “Through this process scars will follow a predictable pattern, appearing red and raised before eventually fading. Patients are advised to avoid sun exposure and wear sunscreen during this period to minimize the risk of hyperpigmentation. Often, the passage of time allows the scar appearance to improve sufficiently to avoid or reduce the need for surgery.”
In general, scar maturation needs to take place in order to assess if reconstructive surgery is in fact needed. The risk of scar problems is also reduced if the surgery is performed after scar maturation. For most burn patients, the average time until the first reconstructive procedure is approximately 1.5 years.
Burn Patient Treatment Options
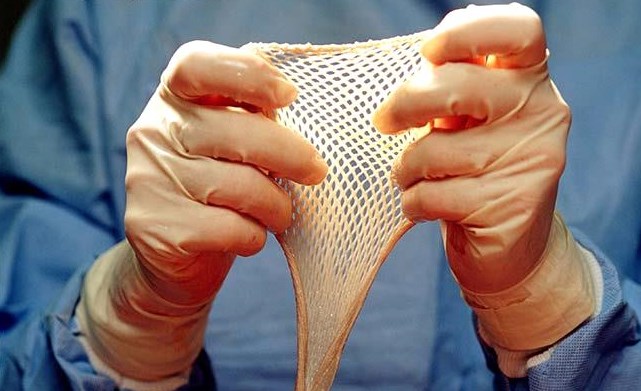
“The most common surgical procedures for burn patients are full thickness skin grafts and split thickness skin grafts,” says Dr. Landon. This is where skin is removed from one part of the body and transplanted to another. “The donor site for skin grafts varies depending on the injury and burn pattern and the presence of additional injuries in which burns are merely a single component of the overall constellation of injuries a patient may have.”
“Typical donor sites include the back of the thigh, the outer edge of the thigh, or the inner edge of the thigh. If more surface area is needed for graft harvest, the front of the thigh can be used, although this will be more noticeable,” says Dr. Landon. “The back also presents a large surface area that grafts can be harvested from. In severely burned patients, your reconstructive burn surgeon will use whatever skin is uninjured for graft harvest. It is always better to have a burn scar from graft harvest, then to succumb to one’s burn injuries due to inability to achieve closure of the burn wounds,” adds Dr. Landon.
Split and Full Thickness Skin Grafts
Skin grafts were first described way back in 1500 BC. Though thankfully, methods have advanced substantially in the past 200 years.
Dr. Ashinoff explains: “Split thickness skin grafts are performed using a device called a dermatome. It allows a predetermined thickness of skin to be “shaved” from the donor site in a uniform manner. The donor site is dressed with Vaseline impregnated gauze and heals via secondary intention. The graft is placed on a healthy wound bed and held in place with a type of pressure dressing.”
As for a full thickness graft, Dr. Ashinoff informs these are “harvested by using a scalpel to excise an ellipse of skin and subcutaneous fat. The donor site is closed directly with suture, the fat is removed from the graft with scissors and the graft is then placed on a healthy wound bed and held in place with a pressure dressing.”
“Once the patient has healed, secondary scar revisions may be considered. These procedures include scar excision, laser resurfacing, contracture release and flaps.”
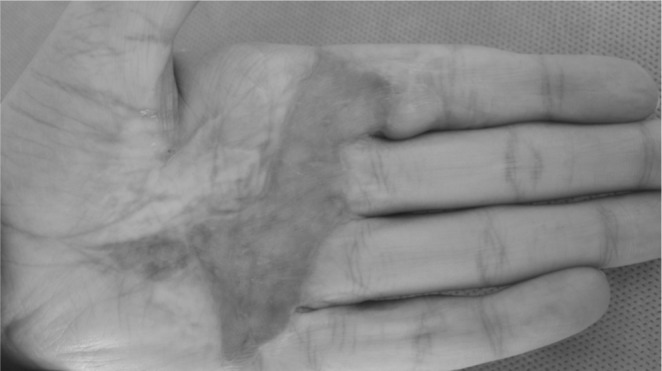
Scar Contracture
Scar contracture is a common complication of burns, occurring in 38-54 percent of patients. A contracture is when the scar pulls the surrounding skin and tissue into contraction, creating a tight scar that limits the patient’s range of motion, making it difficult to perform everyday activities.
Contractures more commonly occur in deep and/or surgically treated burns and are more prevalent on the hands (fingers), neck, elbow and shoulder. Neck contracture can be particularly debilitating.
New scar contractures can appear long after burn injuries occur, especially in young patients who are still growing. Contractures may also affect adjacent joints and muscles. For instance, as a consequence of the contracture, adjacent joints and muscles will be under additional pressure to perform tasks, which can lead to additional problems for the patient.

“Skin grafts are not generally used for treating contracture, as these also tend to contract over time,” says Dr. Ashinoff. “These areas usually require complete excision of the scar followed by resurfacing of the flexion or extension surface. Using adjacent undamaged skin, fascia, or muscle can successfully replace and release the contracture and restore range of motion.”
To accomplish this, Dr. Landon informs that various plastic and reconstructive procedures are used – “Z-Plasty, W-Plasty, local flaps, and even free flaps to bring healthy, uninjured skin from other areas of the body to replace the burned, scarred, contracted skin.”

Your selected plastic surgeon will be able to answer all your questions regarding the best procedures suited to your needs. And thankfully, there is ongoing research occurring that will hopefully see new and improved techniques emerging. A great deal of the research focus is on increasing the tissue expansion of scars and improving the overall cosmetic and functional outcomes for burn injury patients.